1: Smoking and tobacco in Asia
Smoking – a global and regional epidemic
Wherever you sit in the debate about THR, there is no denying the statistics on global smoking are grim. The world’s deadliest non-communicable diseases are directly related to smoking:4
- There were an estimated 1.1 billion smokers globally in 2018.
- Including the use of regional combustible products as well as manufactured cigarettes, the Asia region accounts for around 60% of combustible tobacco users worldwide – a total of 743 million people.
- Half of all those who smoke will die prematurely from smoking-related diseases.
- The Global Burden of Disease (GBD) study estimates that smoking accounted for 7.1 million deaths in 2017, with an additional 1.2 million deaths attributed to second-hand smoking.
- Smoking is the second highest risk factor for death behind high blood pressure, where smoking is also a major risk factor.
- More than half of all annual smoking-related deaths (4 million) occur in Asia – 3 million in China and India alone.
60%
the proportion of the world’s smokers who live in Asia; half will
die prematurely from a smoking-related disease
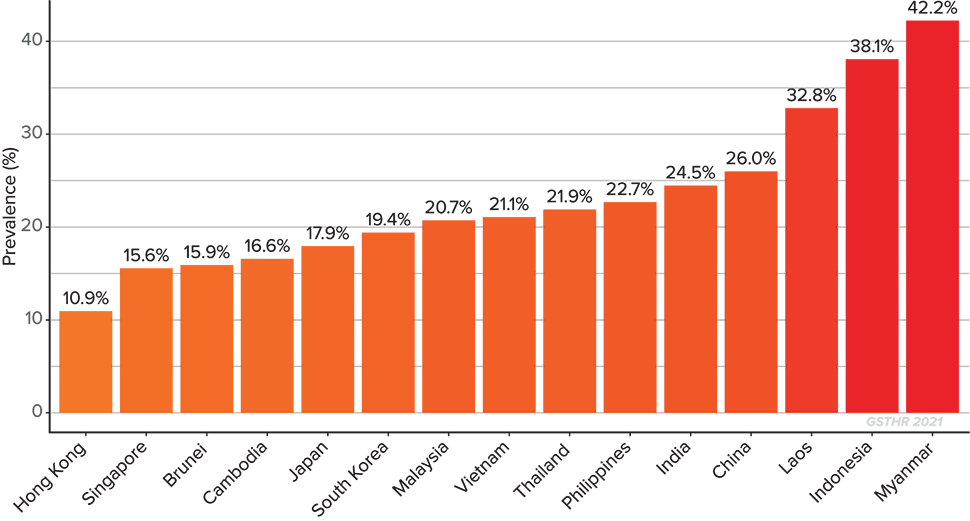
Current adult tobacco smoking rates in Asia
Around one in five adults (19%) in the world smokes tobacco. Most countries in Asia have adult smoking rates in excess of this, and three countries have smoking rates in excess of 30% – Laos, Indonesia and Myanmar.
Current adult tobacco smoking in 2021 in Asia
More than half of all annual smoking-related deaths (4 million) occur in Asia –
3 million
in China and India alone
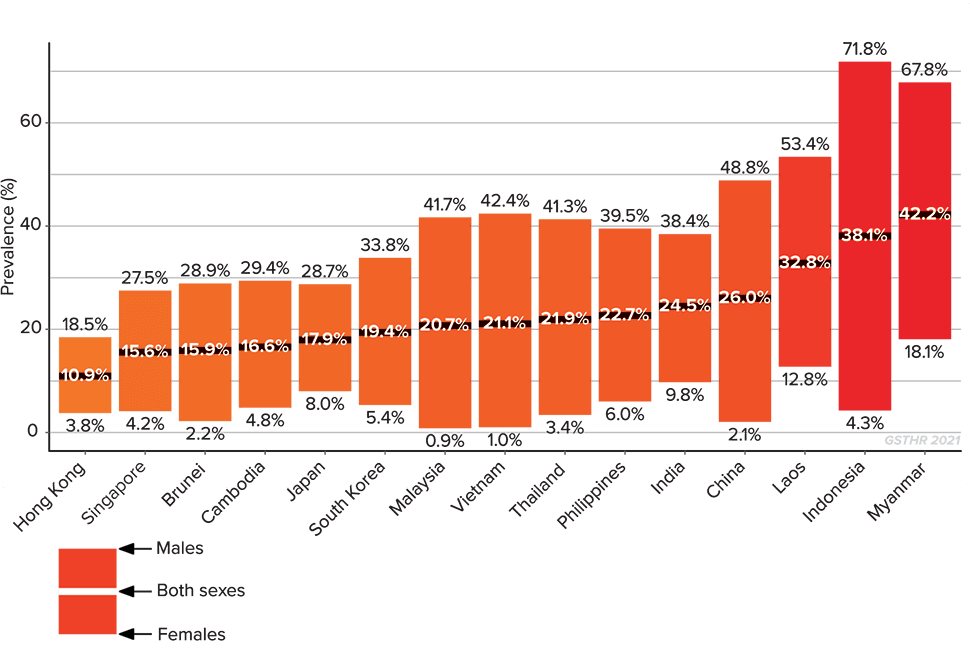
Overall, this region has some of the highest male adult smoking rates in the world. In Myanmar, 67.8% of men smoke. Indonesia has the highest rate of male smokers as a percentage of population in the world at 71.8%. In much of the world, being a non-smoker is the norm for men. In Indonesia and Myanmar, however, by far the majority of men smoke.
Current tobacco smoking in 2021 in Asia
Differences between males and females
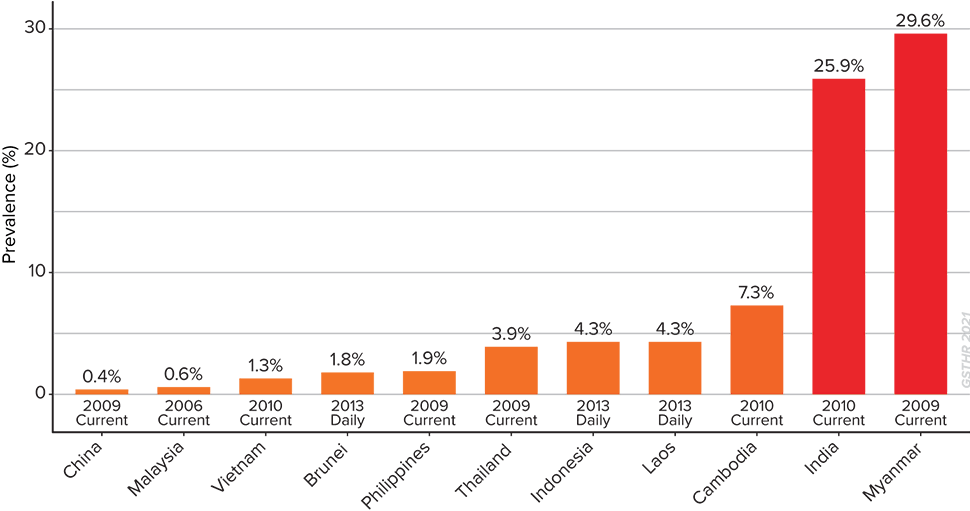
Adult users of smokeless tobacco products5
Two hundred and sixty million people or 89% of the world’s consumers of smokeless tobacco (SLT) live in Asia.
Prevalence of smokeless tobacco use among adults in Asia
89%
the proportion of theworld’s consumers of smokeless tobacco who live in Asia
The region is home to all five of the countries with the highest global prevalence rates of SLT use: Myanmar, Bangladesh, India, Bhutan, and Nepal.
Rural users in India and Bangladesh account for 80% of global SLT users. In India and Myanmar, more men use SLT than smoke cigarettes. In Bangladesh, similar percentages of women and men use SLT while in Cambodia, Malaysia and Vietnam, more women use SLT than men.
Smoking-related death and disease
Every year, over 4 million people in the region die from smoking-related disease – 3 million in China and India alone. In Vietnam, China and Malaysia, more than one in every five deaths is smoking-related.
The Global Burden of Disease (GBD) is published by the Institute of Health Metrics and Evaluation at the University of Washington, USA.6 The GBD analyses 286 causes of death, 369 diseases and injuries, and 87 risk factors in 204 countries and territories.
One metric ranks the 11 major risk factors associated with all death and disease in every country, with the 2019 edition enabling comparisons between 2009 and 2019.
4 million
the number of people who die in Asia annually from a smoking-related disease
In 2009, tobacco was in the top three risk factors for nine of the countries covered by this briefing, while in four countries – China, Japan, Singapore and Thailand, it was ranked number one.
Ten years later, the situation had not improved. And assuming that lung cancer is the cancer most associated with smoking, six out of the same group of countries recorded lung cancer in the top ten list of most prevalent diseases.7
Mortality attributable to smoking tobacco in Asia (% of all deaths)
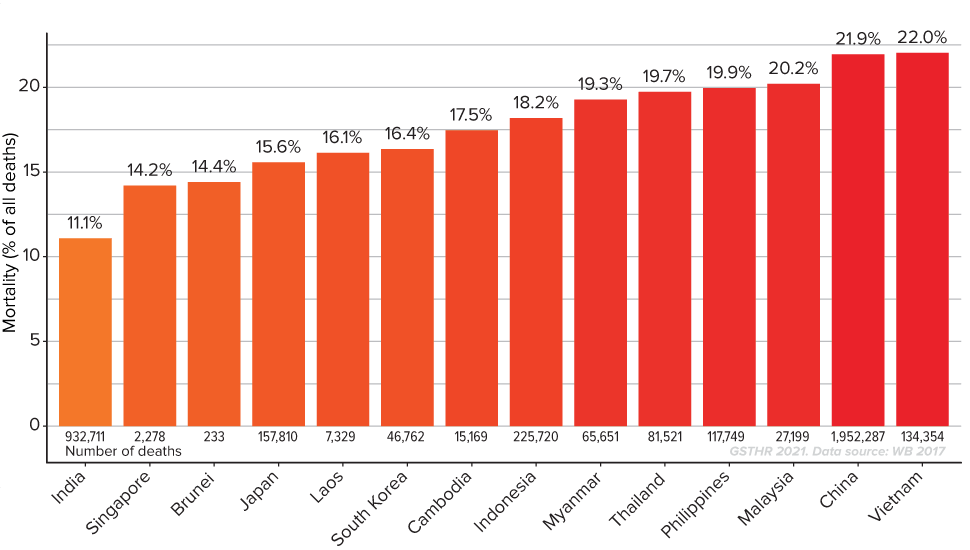
1 in 5
deaths in Vietnam, China and Malaysia is smoking related
Smokeless tobacco-related death and disease
The main way of consuming SLT in the region combines tobacco in a betel quid which is then chewed. Common ingredients are the areca nut, fresh betel leaf and slaked lime paste. There are various names for the product across the region, with a range of additions to the primary ingredients. Apart from Indian gutka, all these chewed products will include tobacco, while there are several regional varieties of snuff-type tobacco products for oral or nasal use.
Four of the five countries with the highest global rates for oral cancer are in Asia
From a public health perspective, the widespread use of these oral products results in the high rates of oral cancer, caused by both tobacco and the areca nut. Four of the five countries with the highest global rates for oral cancer are in Asia: Pakistan, Bangladesh, India and Sri Lanka.8
Help for smokers and smokeless tobacco users
The WHO developed the MPOWER strategy as an implementation tool for the tobacco control measures outlined in the FCTC. The acronym covers the monitoring of tobacco use and prevention policies, protecting bystanders, warning about dangers, enforcing bans and raising taxes. But the most important and most immediate strategy for trying to reduce death and disease from smoking is the ‘O’, which stands for ‘Offering help’. By its own admission, this aspect of the WHO strategy has largely failed. The smokers who need the most help live in countries with the least developed healthcare systems and support services for smokers.
In its 2019 report on the Global Tobacco Epidemic, the WHO admit that 70% of the world’s population have no access to “appropriate tobacco cessation services”. And that even where such services exist, “many countries do not cover the costs of tobacco cessation services for those using them” and “few countries carry out regular monitoring and evaluation that helps improve tobacco cessation services”.9
Regarding nicotine replacement therapy (NRT), the only countries in Asia which claim to fully cover costs are Brunei, Malaysia and India. Yet a study of the availability and affordability of NRT and cessation medicines in the Indian state of Kerala revealed that no products were available in public health care facilities and were only available in some private pharmacies.10
The WHO reported that most countries provided some form of cessation support services. But as few countries have proper monitoring and evaluation processes in place, it is impossible to say how effective these are in terms of numbers attending, quit rates and relapse rates.
However, we do know from studies elsewhere that the relapse rate from NRT is high (whether part of a stop smoking service or not) while counselling services alone are relatively ineffective without other interventions. Using vaping devices as a recognised part of official stop smoking services has proved particularly effective in the UK.11
Even if NRT was readily and freely available in the region, it remains the case that many people who smoke or use SLT do not regard their use of these products as an illness, which limits the success of interventions that are more medical in nature.
Where available, data on quit plans suggests that motivation to quit smoking in Asia is lower than in many other parts of the world. Of the ten countries with the lowest number of smokers intending to quit either in the next month, next year or sometime in the future, six are in Asia.12
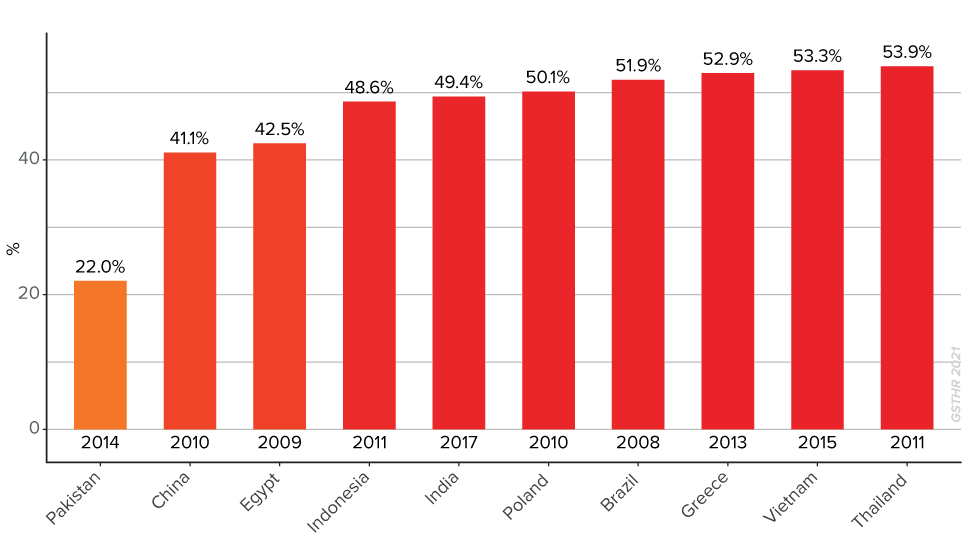
Countries with the lowest proportion of current smokers who intend to quit
In its 2019 Global Tobacco Epidemic report, the WHO devotes several pages to dismissing evidence in favour of the benefits of the use of SNP in reducing the harms from tobacco.13 The WHO has made its position clear that SNP do not serve a purpose as an exit route from smoking. This has had consequences around the world, as governments look for guidance and leadership on regulation or legislation to respond to new products, and consumers look to apparently credible sources of information on how to improve their own health outcomes.
Yet the WHO continues to promote harm reduction interventions in other areas of global health such as HIV and AIDS prevention. Its failure to accept the opportunity offered by tobacco harm reduction is a failure of public health policy of epic proportions. Major progress could be made in reducing the toll of smoking-related death and disease in Asia and worldwide by encouraging smokers and SLT users to switch to safer products while continuing to use nicotine.
Major progress could be made in reducing the toll of smoking-related death and disease in Asia and worldwide by encouraging smokers and SLT users to switch to safer products
- For more comprehensive information on the smoking epidemic, see Shapiro, H. (2020). Burning Issues: Global State of
Tobacco Harm Reduction 2020. Knowledge-Action-Change.
Access full report, p.28: https://gsthr.org/resources/item/burning-issues-global-state-tobacco-harm-reduction-2020
Read the chapter online at https://gsthr.org/report/2020/burning-issues/chapter-1 -
Information and data on smokeless tobacco in this briefing is drawn from: National Cancer Institute and Centers for
Disease Control and Prevention. (2014). Smokeless Tobacco and Public Health: A Global Perspective (No. 14–7983; NIH
Publication). MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National
Institutes of Health, National Cancer Institute.
https://untobaccocontrol.org/kh/smokeless-tobacco/wp-content/uploads/sites/6/2018/06/SmokelessTobaccoAndPublicHealth. pdf - Institute for Health Metrics and Evaluation (IHME) (2019). Global Burden of Disease (GBD 2019). IHME, University of Washington. http://www.healthdata.org/gbd/2019
- Ibid.
- Mouth, pharynx & larynx cancer statistics. (2018, August 22). World Cancer Research Fund.
https://www.wcrf.org/dietandcancer/cancer-trends/mouth-pharynx-larynx-cancer-statistics. Papua New Guinea is the nation with the highest rate of oral cancer. 9 WHO (2019). WHO report on the global - WHO (2019). WHO report on the global tobacco epidemic 2019. Offering help to quit tobacco use. World Health Organization. http://www.who.int/tobacco/global_report/en/, p.45
- Sarma Smitha et al. (2017). Availability, Sales, and Affordability of Tobacco Cessation Medicines in Kerala, India. Circulation: Cardiovascular Quality and Outcomes, 10(11), e004108. https://doi.org/10.1161/CIRCOUTCOMES.117.004108
- McNeill, A. et al. (2021). Vaping in England: evidence update February 2021: a report commissioned by Public Health
England. Public Health England.
https://www.gov.uk/government/publications/vaping-in-england-evidence-update-february-2021 - WHO (2019). WHO Report on the Global Tobacco Epidemic 2019. World Health Organization.
https://www.who.int/tobacco/global_report/en/, p.36 - Ibid., 46–47
