Clearing the smoke: safer nicotine products and health
There is much talk in the media about the vaping ‘controversy’. Smokers, health professionals, policy makers and legislators are understandably confused by conflicting information from what appear to be opposing but equally credible public health, academic and clinical viewpoints.
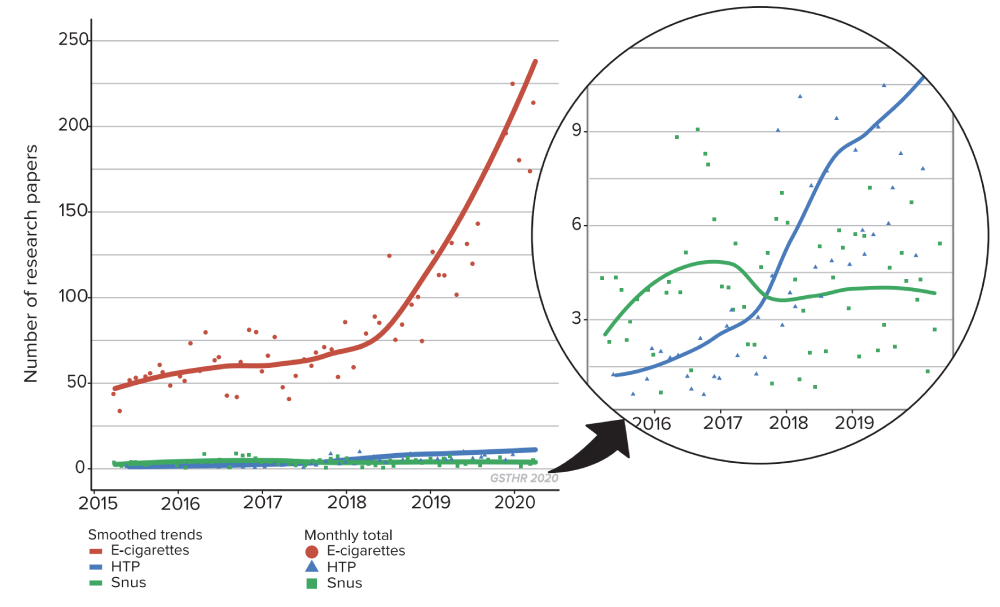
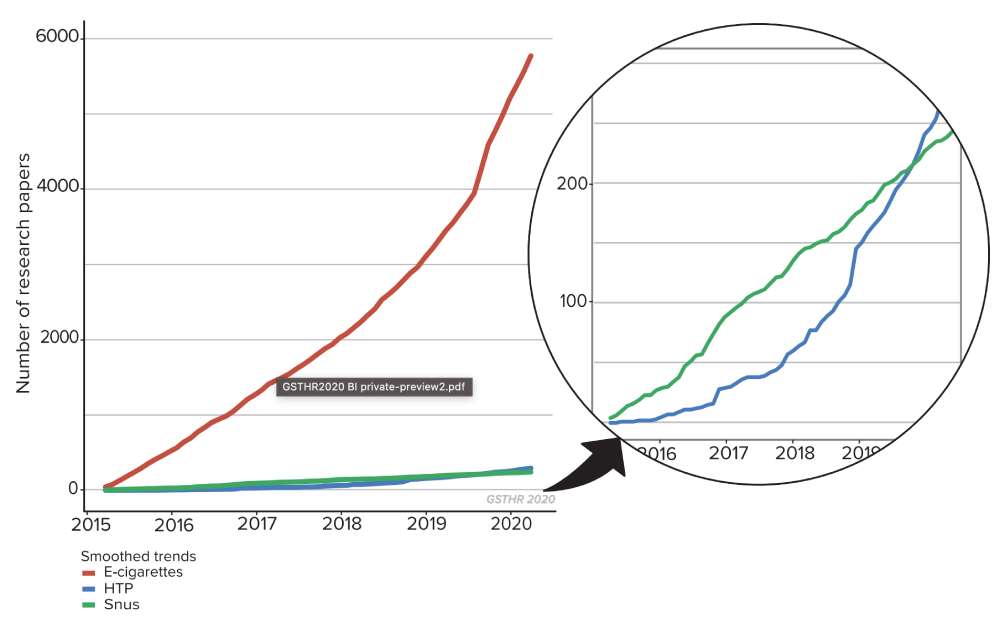
It is often said that little is known about vaping and its products. In fact, there has been a massive expansion in the number of scientific publications on vaping. In the six years from 2007-12, there were only 53 publications recorded. This number grew by 459 in 2015; 751 in 2016; 730 in 2017; 1,023 in 2018; 2,017 in 2019; and 793 up to April 2020, totalling 5,773 publications in peer-reviewed scientific journals. In the seven years from 2013 to 2020, the total covering vaping, HTP products and snus jumped to 6,309. 74
By mid-2020 –
6,309
scientific articles had been published on SNP
There are fewer publications on other SNP. There were only three publications on HTP in 2015; 26 in 2016; 31 in 2017; 90 in 2018; 95 in 2019; and 48 in 2020. In total there were 293 publications on HTP between January 2015 and April 2020.
On snus there were 27 publications in 2015; 61 in 2016; 47 in 2017; 42 in 2018; 53 in 2019 and 13 in 2020. In total, 243 publications on snus from January 2015 to April 2020.
But more science does not always mean better science or better science communication. Poorly formulated and designed research, over-cooked announcements of research results, over-hyped university press releases and an uncritical media with an appetite for bad news stories create confusion among the general public, smokers and users of SNP and health professionals. Taking a balanced view of any issue is not a question of giving equal weight to both sides but making a calculation based on the most robust and credible evidence.
Monthly number of research papers
Cumulative number of research papers
There is also a wider issue of what might be termed ‘nicotine illiteracy’ which goes beyond anti-THR rhetoric: a belief among health professionals and the public that nicotine is carcinogenic.75,76,77
Key points about SNP and health
- There is no such thing as absolute safety. Medicines, whether prescribed or bought over the counter, come with lists of possible side effects and risks.
- The ‘dose makes the poison’. Much depends on the dosage of any substance or the route of delivery into the body. For example, a drug which is injected will reach the brain far quicker than one which is swallowed.
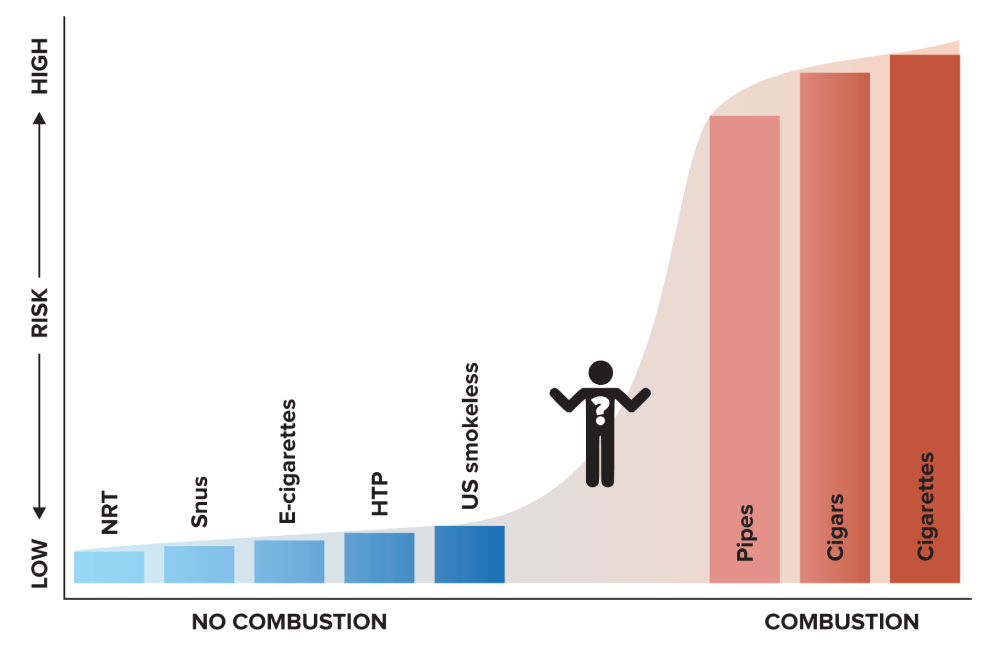
- Vaping and HTP emit substantially fewer toxins than conventional combustible cigarettes, meaning that the potential health risks from smoking are dramatically reduced by switching away from cigarettes. Safer smokeless products, like snus and US smokeless, produce no emissions.
- Most studies only consider the potential absolute health risks of these products – and incidentally find little evidence – rather than looking at the relative risk compared to smoking cigarettes. Relative risk studies focus on reductions in exposures. This doesn’t mean there is no risk, but underlines the key point that the spotlight is on tobacco harm reduction not elimination.
- Someone who has been smoking for decades can enjoy an enhanced quality of life if they switch away from smoking. However, switching or even quitting altogether does not necessarily mean they will not suffer a smoking-related disease at some point, because of the damage already done.
- In relation to long-term effects of vaping products – many people have been vaping for over a decade from all over the world without evidence of ill effects directly and exclusively related to vaping. Just because we don’t know everything, does not mean we don’t know anything.
- No new evidence has appeared since our last report to challenge the best available evidence that using vaping devices, HTP and snus is significantly safer than smoking.
No new evidence has appeared since our last report to challenge the best available evidence that using vaping devices, HTP and snus is significantly safer than smoking.
In the context of tobacco harm reduction – what does ‘safer’ mean?
When a smoker draws on a cigarette, the temperature at the tip rises from about 700 degrees centigrade to 900 degrees – enough to melt metals including aluminium and lead – releasing some 7,000 detected compounds, of which at least 70 are carcinogens. Tobacco is also combusted in cigars, cigarillos and pipes. It is these toxins which create (once water and nicotine are filtered out of the smoke) tar, which is one of the main factors contributing to cancer and other cardiovascular and respiratory diseases. No other way of consuming nicotine comes close to the dangers posed by smoking, as the chart below shows.
No other way of consuming nicotine comes close to the dangers posed by smoking.

Continuum of risk for nicotine containing products
“Vaping poses only a small fraction of the risk of
smoking and switching completely [...] conveys substantial health
benefits.”
– Public Health England, 2020
Regarding vaping devices and based on a comprehensive evidence review, Public Health England (PHE) confirmed in its 2020 report their earlier conclusion that:
“Vaping poses only a small fraction of the risk of smoking and switching completely from smoking to vaping conveys substantial health benefits over continued smoking. Based on current knowledge stating that vaping is at least 95% less harmful than smoking remains a good way to communicate the large difference in relative risk so that more smokers are encouraged to make the switch from smoking to vaping.”78
With HTP, the situation is slightly different because tobacco is involved and is heated (at different temperatures depending on the device) although never above 350°C, and so below the combustion temperature of cigarettes. It is crucial to demonstrate that no combustion occurs with HTP. This can be done by showing that the devices work in the absence of oxygen. An independent assessment, conducted for New Zealand’s Ministry of Health, confirmed that no combustion occurs in the heated tobacco product IQOS when used as intended.79
PHE and the UK Committee on Toxicity, Carcinogenicity and Mutagenicity of Chemicals in Food, Consumer Products and the Environment considered the available evidence in 2017.80 The UK Committee on Toxicity (COT) highlighted significant reductions in levels of harmful and potentially harmful constituents (HPHCs) in the aerosol of HTP compared to cigarette smoke and stated that “[t]here would likely be a reduction in risk for conventional smokers deciding to use heat-not-burn tobacco products instead of smoking cigarettes.”81 COT added that “[a] reduction in risk would also be experienced by bystanders where smokers switch to heat-not-burn tobacco products”. 82
Most of the scientific and clinical literature on HTP has been provided by the industry. However, the body of independent research on these products is growing. In 2018, PHE reviewed 20 extant studies (12 of which were the product of tobacco company research) and reiterated these points based on the available evidence and noted the potential of HTP: “Compared with cigarette smoke, heated tobacco products are likely to expose users and bystanders to lower levels of particulate matter and harmful and potentially harmful compounds. The extent of the reduction found varies between studies. […] The available evidence suggests that heated tobacco products may be considerably less harmful than tobacco cigarettes and more harmful than e-cigarettes.”83 Independent analytical chemistry studies on HTP have confirmed manufacturers’ findings showing that HTP products generate much lower levels of harmful constituents compared to tobacco cigarettes.84,85,86 A review of studies of likely daily exposure indicated that cancer risk from HTP is between one and 10 per cent that of cigarettes.87 A comprehensive independent review looked at the evidence from 31 studies, including eight that were not industry-based, but all of which were peer-reviewed, concluding that devices delivered up to 75 per cent fewer harmful toxins and overall that HTP “expose users and bystanders to substantially fewer harmful and potentially harmful compounds than smoking cigarettes”.88
“Based on current knowledge stating that vaping is at least
95% less harmful than smoking remains a good way to communicate
the large difference in relative risk so that more smokers are encouraged
to make the switch from smoking to vaping.”
– Public Health England

The evidence on smokeless products
US smokeless89
It has been known for almost three decades that those who avoid smoking cigarettes – known as chewers and dippers and those who use snus – eliminate about 98 per cent of the risks associated with smoking.90 The risks are so small that even large epidemiologic studies with hundreds of thousands of users cannot provide indisputable evidence that smokeless tobacco (ST) causes any specific disease.91 With risks that small, it is not possible to prove that one kind of dip, chew or snus is safer than the other92.
Decades of scientific studies document that ST use is vastly safer than smoking with respect to cancer,93 heart attack and strokes94 and many other diseases. In 2002, a report by the Royal College of Physicians stated, “As a way of using nicotine, the consumption of non-combustible [smokeless] tobacco is in the order of 10–1,000 times less hazardous than smoking, depending on the product.”95 In 2008, the American Association of Public Health Physicians became the first medical organisation in the US to formally adopt a policy of “encouraging and enabling smokers to reduce their risk of tobacco-related illness and death by switching to less hazardous ST products.”96
The risks are so small that even large epidemiologic studies with hundreds of thousands of users cannot provide indisputable evidence that smokeless tobacco (ST) causes any specific disease.
The Global Burden of Diseases, Injuries and Risk Factor Study provides a comprehensive assessment of risk factor exposure and attributable burden of disease. For example, the 2016 study states:
“for the first time in the GBD study, we estimated exposure to and burden attributable to smokeless tobacco… RR [Reduced Risk] estimates were derived from prospective cohort studies and case-control studies… Based on available evidence, for chewing tobacco, RRs were significantly higher than one for oral cancer and oesophageal cancer, while for snus or snuff we did not find sufficient evidence of an RR greater than one for any health outcome”.97
Snus
The use of snus in Sweden provides a real-world proof of concept for THR using SNP and one that could potentially deliver significant benefits in those regions where more dangerous smokeless products have become culturally embedded.98

Snus use in Sweden is high compared to smoking, enabling the country to enjoy the lowest rate of smoking-related mortality in Europe and half the average EU rate for smoking-related disease. The low levels of smoking mean there are low levels of respiratory disease linked with inhalation. Additionally, the epidemiological evidence is that snus is not associated with diabetes, oral and pancreatic cancers, or cardiovascular disease. 99,100,101,102,103,104
In its 2008 investigation, the EU Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR) reported several conclusions about the health effects of ST and snus. Significantly, it found that complete substitution of ST for tobacco smoking would ultimately prevent nearly all deaths from respiratory disease currently caused by smoking and reduce the cardiovascular mortality that currently arises from smoking by at least 50%. They also concluded that there was no obvious gateway effect from snus to cigarettes among young Swedish people.105
[An EU scientific committee found that] complete substitution of ST for tobacco smoking would ultimately prevent nearly all deaths from respiratory disease currently caused by smoking.
US lung injuries and deaths: mistakes, miscommunication and misinformation106
A key health issue that has arisen since our 2018 report was the outbreak of serious lung injuries and deaths in the US.
From around March-April 2019, cases of lung disease (cough, shortness of breath, difficulty breathing, fatigue and vomiting) emerged in Illinois and Wisconsin with a rapid increase in reporting occurring in August and September across the US. The first death occurred on 23 August 2019. As of March 2020, just under 3,000 people had been hospitalised with around 70 deaths. There have been no confirmed deaths outside the US.
Early official public health reporting called the outbreak ‘e-cigarette’ or vaping product associated lung injury or EVALI, leading many to believe that conventional nicotine vaping products were responsible. It soon became clear that a more appropriate name would have been vitamin E-related lung injury or VITERLI because the substance doing the damage was vitamin E acetate. This oil-based substance has never been detected in ordinary nicotine e-liquid, which is water-based.
People affected by VITERLI were inhaling vaporised cannabis (THC) oil to which vitamin E acetate had been added to give the appearance in texture and colour of a highquality oil in illicitly manufactured THC cartridges. Some of those hospitalised initially claimed they had been vaping nicotine liquid, but subsequent questioning and testing found substantial under-reporting of marijuana, likely due in part to use still being illegal in many parts of the US.107 The cannabis website Leafly charted the causes of the outbreak and first exposed the multi-billion dollar industry producing and selling illicit THC oil and fake THC vaping devices and associated accessories.108,109,110

Credit: David Downs Leafly
The Centre for Disease Control (CDC) VITERLI timeline111
To the astonishment of many vapers and THR professionals, in 2020 the CDC lung injury team was nominated for a Service to America award for its response to the outbreak. By contrast, many critics thought that the CDC took advantage of its existing opposition to vaping to spread fear and misinformation. Media reporting in the US and around the world “contributed to regulatory overreactions to nicotine vaping by the public health community”.112 This misreporting continued even after the CDC finally revealed that the vaping of illicit THC was causing the deaths and injuries.113
25th July: Wisconsin Department of Health Services sends a memo to healthcare providers concerning severe pulmonary disease among adolescents who reported vaping and other ‘inhalant drug use’. Types of products used were unknown and patient interviews ongoing.
12th August: California Department of Public Health issues an alert to the effect that “reported common exposure among these patients is that they have been vaping cannabis or cannabidiol (CBD) oils. At this time, no infectious cause has been identified.”
23rd August: Brian King of the CDC Office on Smoking and Health tells reporters:
“…there’s a variety of harmful ingredients identified [in nicotine vaping products], including things like ultrafine particulates, heavy metals like lead, and cancer-causing chemicals. And flavoring used in e-cigarettes to give it a buttery flavor, diacetyl, and it’s been related to severe respiratory illness. That being said, we haven’t specifically linked any of those specific ingredients to the current cases, but we know that e-cigarette aerosol is not harmless.”
Meanwhile there had been 193 acute lung injury cases and 1 death. In all cases, illicit THC oil cartridges had been identified as the specific product most likely responsible.
28th August: USA Today reports: “People are vaping THC. Lung injuries being reported nationwide. Why is the CDC staying quiet?”
5th September: New York Times reports that, “The state said that the Vitamin E compound was found in tests of cannabis products, but not in the nicotine-based products it tested, a finding consistent with reports from doctors that many illnesses have been linked to people using a vaping device for marijuana.”
6th September: Despite the growing body of evidence about the true cause of the outbreak, the CDC tell the Washington Post that when it came to clinical tests, ‘‘We don’t know what we’re looking for”.
4th October: Tentative FDA warning not to vape THC.
25th October: Despite 33 deaths directly linked to vaping THC, the CDC tell reporters, “We recommend that you do not use e-cigarette, or vaping, products that contain THC. And since the specific compounds or ingredients causing lung injury are not yet known, the only way to be sure that you are not at risk is to consider refraining from use of all e-cigarette, or vaping, products while our investigation continues.”
8th November: New York Times reports that the CDC has finally linked the illnesses and deaths to vitamin E. However, allegations against nicotine vaping products continue: “Nicotine has not been exonerated… Some patients say they vaped only nicotine, and state health officials consider some of those reports reliable”.
25th February: CDC says that “... Adults using nicotine-containing e-cigarette, or vaping, products as an alternative to cigarettes should not go back to smoking... If they choose to use e-cigarettes as an alternative to cigarettes, they should completely switch from cigarettes to e-cigarettes and not partake in an extended period of dual use of both products that delays quitting smoking completely...”. 114
Writing for Leafly, David Downs and colleagues estimated that 78 per cent of the US THC vaping business is outside any regulation or control – starkly revealed when the authors had some residual oil from one VITERLI victim tested by SC Labs, an accredited California- based facility specialising in cannabis product testing. The lab not only found vitamin E, but also lead and pesticides in “insane concentrations”, to quote SC Lab President, Josh Wurzer.
How does vitamin E specifically cause damage? Vitamin E acetate disrupts the function of the lungs’ fluid lining, impeding oxygen transfer, and triggering a progressive and severe immune reaction. Some reports indicate a person’s lungs can begin to lose function as quickly as a week after exposure to THC oil heavily cut with vitamin E acetate.
“When you inhale this fatty substance, it sort of acts like a soap,” said Wurzer. “When it gets in your lungs, it breaks up all the surface chemistry that’s happening with your lungs and really interferes with the exchange of oxygen into your bloodstream.”
[The evidence] did not prevent US anti-THR activists, federal agencies and politicians using the VITERLI outbreak as a way to further their agenda and call for bans.
Local public health authorities identified the root cause of the problem from the outset. This did not prevent US anti-THR activists, federal agencies and politicians using the VITERLI outbreak as a way to further their agenda and call for bans. A lesson to be learned is that banning products already in wide circulation allows a criminal market in unregulated and potentially dangerous products to step in.
Is there evidence that vaping increases the risk of lung and heart disease?
Health concerns about nicotine vaping products focus on the effects of vapour constituent deposits in the mouth, upper airway and lungs and the overall effects on bodily functions of vapour inhalation.115 These constituents include nicotine, propylene glycol, glycerine and flavours.
Nicotine is a psychoactive substance, but at commonly used dose levels, short-term nicotine use does not result in clinically significant harm116 while the long-term adverse effects are also likely to be minimal.117,118
According to the International Agency for Research on Cancer (IARC) nicotine is not a carcinogen119 and a US Surgeon General’s report concluded nicotine does not contribute to respiratory diseases.120
Tobacco smoke and vapour follow the same pathway into the mouth and upper airway, through the gastrointestinal tract and are then excreted. The deposit and absorption of smoke-derived carcinogens increase the cancer risk impacting on various organs but, given the very low level of potential carcinogens in vapour, the risk – either relative or absolute – is low.
There is the possibility of vapour-induced lung irritation and the attendant increased risk of adverse respiratory impact in people with hypersensitivities to certain chemicals. However, many smokers who switch report improvements in lung function.121,122 A study by Jacob George and colleagues concluded that consumers of vaping products, especially women, “demonstrate significant improvement in vascular health within 1 month of switching [from smoking cigarettes to vaping]”.123
Regarding propylene glycol in vaping products, apart from possible minor irritation, there are no other known harmful effects, while animal studies have failed to demonstrate harmful effects on the lungs of inhaling glycerine. Lower incidence of airway infections of smokers who had switched to vaping products has been reported.124,125
A widely-cited study claimed to have detected an excessive presence of metals in vapour.126 However, the authors evaluated the exposure to metals in vapour in terms of total air breathed on a daily basis, when vapers are only exposed while vaping, which is typically 150–200 four- to six-second puffs per day, that is, an exposure of 12–16 minutes per day.127
Concerns have been expressed about the safety of some ingredients used in creating flavours. These are industry standard ingredients for oral consumption in food, but can be risky when inhaled, including diacetyl and acetyl propionyl (used in sweet/buttery flavours), although there are other safer compounds producing a buttery flavour.128 There has been much media coverage of a condition known as ‘popcorn lung’ (bronchiolitis obliterans), suffered by employees working in popcorn factories who have been exposed to high levels of this compound.
The symptoms, such as coughing, shortness of breath and wheezing, might be indistinguishable from the effects of long-term smoking in a vape consumer who had switched, although exposure levels would be several orders of magnitude lower than a factory environment. This respiratory condition has never been reported in vapers. Even so, manufacturers are now avoiding flavours that contain diacetyl: in the EU it is now banned. There has been some debate about cinnamon flavours (which cannot be reproduced using anything but cinnamaldehyde), but evidence again suggests this is primarily an occupational health issue in the factory environment where large quantities are used.
Other chemical components in vaping liquids are generated when the liquid is heated, including formaldehyde and acrolein, while the device and the device elements can also release aerosolised particles of metal, ceramic and rubber when heated. Exposure is well below recognised safety thresholds but could be reduced still further by improved manufacturing standards.129
A 2017 study by Dr William Stephens from the Department of Earth and Environmental Studies at St Andrews University in Scotland calculated that vaping has 0.4 per cent of the cancer risk of smoking (99.6 per cent risk reduction).130,131
The new pandemic: nicotine, vaping, smoking and COVID-19
Following hard on the heels of the lung-injury scare, those opposed to THR were only too keen to launch warnings linking vaping to more severe outcomes or susceptibility to COVID-19.
A few studies have shown an association between vaping and lung inflammation which led some to suggest that vapers might be more susceptible to COVID-19. These studies were the result of exposing cell cultures or rats, or small samples of vapers who were invariably ex- or current smokers, to vapour. Longitudinal studies studying vaping in real world situations have not replicated laboratory studies in respect of vaping and lung inflammation or infections.132
Moreover, early research has suggested that nicotine could be a protective factor against initial COVID-19 infection and disease progression meaning that smokers are less likely to test positive for COVID-19133 and less likely to be admitted to hospital but, if admitted, have worse outcomes. This has led to a theory that nicotine could be a protective factor as the person would no longer have access to nicotine.134,135,136,137
The hypothesis of the protective effect of nicotine is based on (1) the possibility that the interaction of nicotine with nicotinic receptors in the brain might inhibit the proteins that allow the virus to attach to cells and (2) the possibility that nicotine could inhibit the over-reaction of the immune system (the so-called cytokine storm) that in most cases ends up producing massive lung inflammation that overwhelms and kills very ill patients.
To our knowledge, there is no data on vaping status in any of the many published studies on hospitalised or seriously ill COVID-19 patients. It is highly likely that in the chaos of the pandemic, doctors asked patients about smoking status (as they are well used to doing, especially in respiratory care), but that they may not have asked about vaping. This lack of data is problematic for our understanding of any potential interaction between susceptibility to and progress of COVID-19 and vaping status; it is also extremely difficult to disaggregate health impacts that relate to past smoking or present vaping. The medical profession should be encouraged to ask all COVID-19 patients about current and past smoking status and current and past vaping status in order to get the fullest possible picture – which may yet take some considerable time to emerge.
Second-hand vapour is not the same as second-hand smoke
Vaping devices emit ‘vapour’, a mist-like aerosol. The user absorbs about 90 per cent of the inhaled vapour (86 per cent of glycerol, 92 per cent of propylene glycol, 94 per cent of nicotine and 97 per cent of aldehydes).138,139
The exhaled vapour released into the environment is an extremely diluted aerosol whose gas phase is propylene glycol, glycerol and water vapour, with residual doses of pollutants (aldehydes). There are misleading mentions in environmental studies about the presence of harmful fine and hyper fine ‘particles’ in this aerosol, creating concerns by equating them to suspended particles of air pollution or cigarette smoke.140
However, the ‘particles’ in exhaled (and inhaled) vapour are liquid droplets whose chemical composition closely matches the composition of e-liquids: propylene glycol, vegetable glycerine, nicotine and water.141 These droplets evaporate and disperse in seconds142,143 and are completely unrelated to suspended particles of air pollution or cigarette smoke (which are produced by combustion processes). They pose minimal risk to bystanders.144,145

“To date, there have been no identified health risks of passive vaping to bystanders.” – Public Health England
However, large clouds of vapour can cause concern among passers-by who might equate this with cigarette smoke and be concerned about the possible effects of their own inhalation. Large clouds of vapour, for example, when many vapers are vaping high powered devices, can irritate the throat in enclosed spaces, (incidentally, this does not occur with low powered devices or when only one or two vapers are vaping). Many vapers are reasonably discreet about their use, adopting ‘stealth vaping’, by inhaling less vapour and holding it in.
To quote PHE: “To date, there have been no identified health risks of passive vaping to bystanders”146 – a view underlined by other recent studies.147,148
Young people and vaping
The arrival of JUUL on the US market has been another major vaping-related news story since our last report, with exaggerated claims of a teenage ‘vaping epidemic’ prompting knee-jerk flavour bans across the US and elsewhere.
Changes in the prevalence of smokers and vapers among American youth
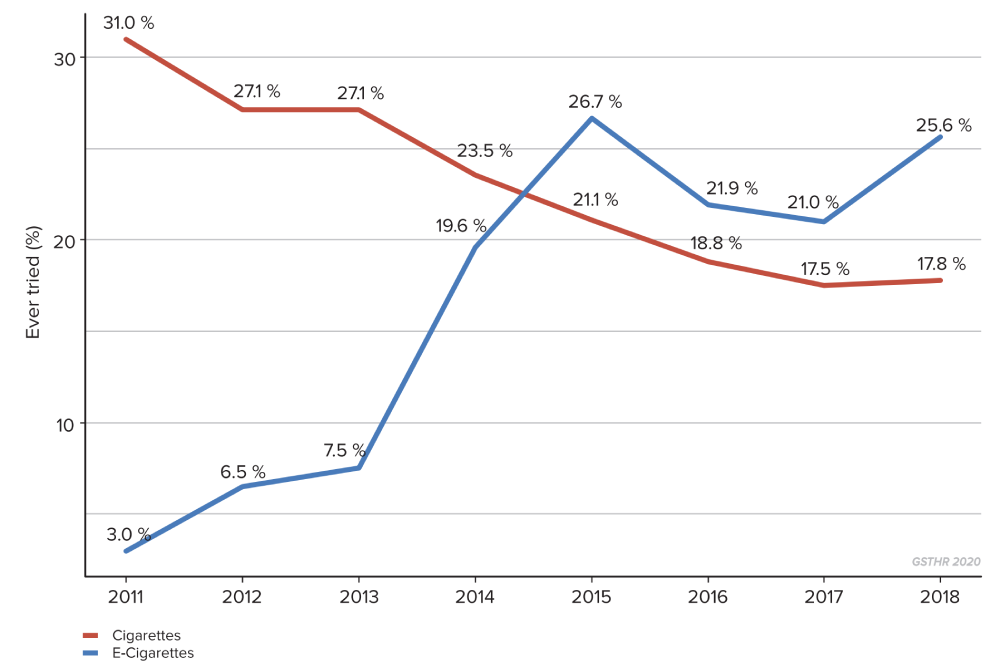
Cigarette smoking has been falling in the US for many years including among young people. When vaping products began to appear on the market, it was inevitable that some young people would want to experiment. This led to claims from the FDA, the Campaign for Tobacco Free Kids (CTFK) and others that vaping was a gateway to smoking as the industry tried to compensate for falling numbers of younger smokers by promoting new products. Yet as the graph shows, cigarette smoking among young people has continued to fall, even while experimentation with vaping devices has been increasing. The goalposts shifted; the claim now from the same bodies is of a vaping “epidemic” among young people which would lead to a future generation of nicotine “addicts”. JUUL certainly attracted a lot of interest from some young people when it launched during 2018-19, while the company itself faced accusations of marketing the device to young adults and selling flavours that appeared to be targeting that same younger audience.
The public, the media and legislators continue to be misled over the prevalence of vaping among young people by the simple trick of conflating ‘ever use’, which could be just once or very infrequent, with ‘use’.
However, a study by Allison Glasser and colleagues from New York University (NYU) College of Global Public Health looked at the 2018 National Youth Tobacco Survey of 20,000 middle and high school students and concluded that:
Most youth who do vape are current or former smokers and many are also vaping THC.

Data from the UK ASH revealed a similar picture of occasional use with few younger teenagers vaping and even fewer vaping who had never previously smoked.151
While it might be preferable for young people not to vape, from a health point of view, it is preferable that if young people are going to consume nicotine, better they vape than smoke. The NYU researchers also discovered that over 40 per cent of those students who vaped also smoked cannabis. This research and other studies point to what are called ‘shared risk factors’ linking vaping, smoking and the use of cannabis among young people.152,153,154
Some commentators have claimed that nicotine has a deleterious effect on adolescent brains, causing hitherto unnoticed long-term damage, reducing test scores and inhibiting life chances. If there was any evidence of nicotine-related brain damage in young people, it would have been noted over the many decades of smoking research.155
If there was any evidence of nicotine-related brain damage in young people, it would have been noted over the many decades of smoking research.
Options for smoking cessation
Many people quit smoking without recourse to professional help or medical products. Others may combine a range of interventions in a bid to end their smoking habit. Availability of and access to these interventions differs significantly between countries, national health systems and individual socioeconomic status.
Nicotine replacement therapy (NRT)
NRT first appeared in the US in 1984 and over time, various products have come onto the market: patches, chewing gum lozenges, sprays and inhalers. NRT is included in the WHO Essential Medicines List. The principle behind them is that they replace the nicotine, while the smoker perhaps engages with a counselling or stop smoking service for behavioural help in quitting cigarettes.156 Using more than one NRT product plus counselling within a stop smoking service has been shown to be more effective than just buying NRT at the pharmacy with no other support. NRT products are produced by the pharmaceutical industry; lead players include Pfizer, Novartis, Cipla, Johnson and Johnson and GlaxoSmithKline.


Pharmaceutical products
There are two main pharmacotherapeutic options; varenicline (marketed as Champix and Chantix) and bupropion (marketed as Zyban and Wellbutrin). Unlike NRT, these drugs aim to suppress the nicotine craving. Champix works by interfering with nicotine receptors in the brain, preventing the person both from experiencing pleasure and suppressing nicotine withdrawal symptoms. Zyban was initially used to treat depression in patients and also works by diminishing the chemicals in a person’s brain that are responsible for cravings and withdrawal symptoms. As with any drugs, both come with a range of possible side-effects and contra-indications.

There are a several ways out of smoking and people will use a combination of interventions. But for many, these options do not work or do not work over time. For most, the reason is that NRT and drugs do not replicate the smoking experience, and ‘medicalise’ smoking, which many smokers find unacceptable. Smokers do not necessarily regard themselves as ‘ill’ simply because they smoke.
Overall, the relapse rates from smoking remain high. As O’Leary and Polosa point out, even for those who do quit smoking, relapse is the norm. For unsupported quit attempts, 80 per cent relapse in the first month and for smokers undergoing treatment, 75 per cent fail within six months, with the large majority resuming smoking within two weeks. The same high relapse rates occur in women in pregnancy and post-delivery and either gender on being discharged from hospital. Even a successful one-year quit does not ensure that abstinence has been achieved as 30 to 40 per cent of former tobacco smokers will eventually relapse. “Consequently, there is a pressing need for alternative and more efficient means to reduce or prevent harm in those who return to smoking”.157
As a UK ASH/Cancer UK report noted, stop smoking services in England are under funding threat,158 but they are also seeing fewer people since the advent of vaping devices. This suggests that vaping is an easier off ramp to navigate away from smoking than other methods, whose aim is solely quitting. So how does NRT compare with vaping when both are used in conjunction with behavioural support in a stop smoking service?
Peter Hajek and colleagues undertook a study whereby nearly 900 smokers who wanted to quit were randomly assigned to NRT or vaping devices plus counselling. The trial ran from 2015–2018 with a one-year follow-up.159 They found:
“Smokers using e-cigarettes suffered less cigarette withdrawal discomfort early on and had higher quit rates at all time points. At 1 year, 10 per cent of participants in the NRT trial arm had been abstinent for the whole year compared with 18 per cent in the e-cigarette arm; regarding abstinence for at least 6 months, the figures were 12 per cent in NRT and 21 per cent in the e-cigarette arm. Of interest, coughs and phlegm production also reduced more in people quitting with e-cigarettes, than those quitting with NRT. This supports previous reports that an ingredient in e-cigarettes (i.e. propylene glycol) may protect vapers from airborne infection. E-cigarette starter packs cost much less than NRT and so if SSS (stop smoking services) provide them, their use is likely to boost the success rates and reduce the costs of SSSs.”
“Smokers using e-cigarettes suffered less cigarette withdrawal discomfort early on and had higher quit rates at all time points.”
Low and middle- income countries
As we have outlined, it is LMIC which bear the brunt of the smoking epidemic. Smokers in these countries would be better served if health professionals felt confident to recommend SNP options for those who want to quit smoking. Unfortunately, doctors are being advised against encouraging these options, by researchers and NGOs often from high-income countries, peddling misinformation about the dangers of SNP.160

Therefore, doctors in LMIC are being advised to stick to approved cessation medications when the health systems in many of these countries cannot afford to buy them. Smitha Sarma and colleagues conducted a survey in Kerala, India, and found smoking cessation medications were not available in public hospitals and even in those services offering cessation services. They were only partly available in private and semi-private pharmacies, meaning the poorest people with more acute problems were denied access.161 As the majority of tobacco users in India do not smoke industry cigarettes but local varieties, including smoke-free products, this suggests that the ready availability of affordable snus-style smokeless products could have significant beneficial health impacts, not only across India but also other countries in the region with similar tobacco-using profiles.
Cessation of smoking using SNP in pregnancy
The harms of smoking during pregnancy include low birth weight, pre-term delivery, increased risk of malformations, respiratory disease and childhood cancers. Cigarette smoke carries all the risks, so it is reasonable to assume that smokeless products carry less risk. The most recent study looking at this issue comes from Glover and Phillips162 who reviewed the evidence on pregnancy outcomes and smokeless tobacco products.
They identified an initial tranche of 500 studies of which only 21 passed muster to be included. Of the 21 studies reviewed, 12 reported on the use of nicotine replacement therapies, seven on Swedish snus, one on Alaskan iq’mik,163 and one on vaping products.

The authors contend that it is not possible to give pregnant women definitive advice on safety, except to say the use of smoke-free nicotine products will almost certainly have less effect on pregnancy outcomes than smoking. They also conclude that if a pregnant woman would otherwise smoke, there is no evidence to deny her access to smoke-free products.
This is similar to the conclusions of the UK’s Royal College of Midwives, whose position statement on support for smoking cessation during pregnancy stated:
- “E-cigarettes contain some toxins, but at far lower levels than found in tobacco smoke. If a pregnant woman who has been smoking chooses to use an e-cigarette (vaping) and it helps her to quit smoking and stay smoke-free, she should be supported to do so.”
- “If a woman has switched completely to vaping and is not smoking at all, she should be recorded as a non-smoker.”
- “Based on the available evidence on e-cigarette safety, there is no reason to believe that use of an e-cigarette has any adverse effect on breastfeeding. ‘Vaping’ should continue if it is helpful to quitting smoking and staying smoke free.”164
Nicotine and addiction
The focus on addiction to nicotine as the main risk to young people has gained ground since the last report.
The illustration is a collage of pre-Second World War American newspapers. It shows that in the hands of the supernatural ‘drug fiend’, drugs like cocaine and heroin become disease vectors, infecting young people with the virus of addiction and – ultimately – destroying their lives.
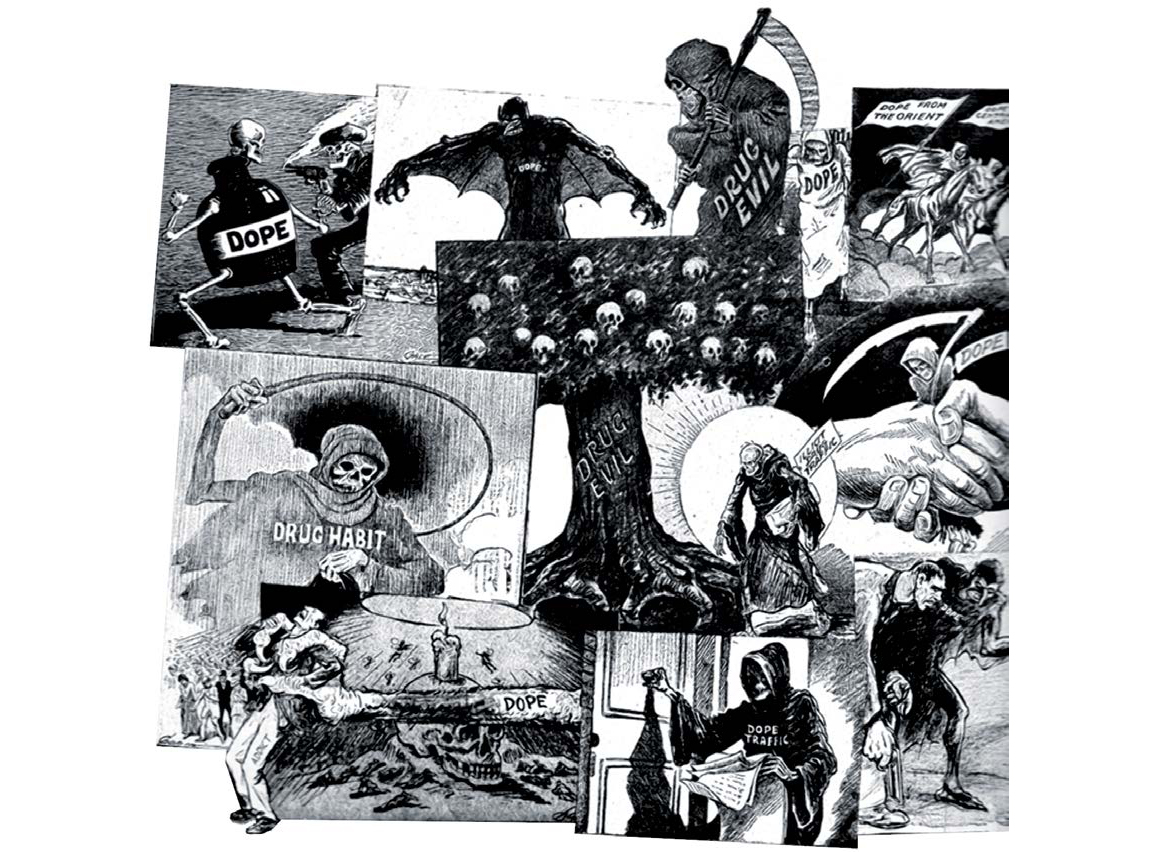
Dependency on drugs like cocaine and heroin can and does destroy lives. But this does not apply to nicotine. Yes, lives can be destroyed by smoking and the deaths and disease it causes – but as millions of consumers of SNP around the world would testify, lives have not been destroyed by nicotine, neither physically nor mentally.
The meaning of addiction
Addiction is an ill-defined concept which has been applied to many substances and activities; the whole range of psychoactive drugs, both legal and illegal; gambling; shopping; sex; eating; or playing computer games.
When deemed to be out of control and adversely affecting other areas of life, all these are classified by the medical profession as psychiatric conditions. From a commonsense, real-world point of view, however, there is a clear difference between injecting heroin and buying inordinate pairs of shoes.
In the case of nicotine, from a neuro-biological standpoint, it is a mild stimulant drug which binds to the equivalent receptors in the brain like a key fitting into a lock. Once locked in, nicotine stimulates the release of the neurotransmitter dopamine which is crucial to the reward and reinforcement effects that constitute the drug experience.
Simply put, dopamine could be called ‘the good time chemical’; it is responsible not just for the pleasure people derive from intoxication,165 but also for sexual gratification and the satisfaction of eating, without which humans would die out.
The influence of the senses and the environment
As the Royal College of Physicians report pointed out, however, the rewards and reinforcement of smoking are not just about the specific drug/brain interaction, although of course, the brain has a role to play in all our sensory experiences:

“Continued pairing of the rewarding/reinforcement pairing with specific and sensory and environmental stimuli (which for example, could include the smell of tobacco or the sight of a packet of cigarettes) results in these stimuli also acquiring reinforcing properties.”166
This could also involve certain rituals like the first cigarette in the morning, or always having a smoke with a drink or a meal.
Varied interpretations of addiction
From that point of view, nicotine is ‘addictive’; people say they crave cigarettes, get ‘withdrawal symptoms’, feel agitated and irritable and find it hard to concentrate if they run out.
Influenced strongly by the psychiatric and rehabilitation industries, addiction is viewed in society as a disease caused by the brain being ‘hijacked’.
Yet ‘addiction’ to nicotine falls far short of the addiction criteria set out in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (2013), the gold-standard text on the names, symptoms and diagnostic features of recognised mental illnesses. Here, the features of addiction include taking the substance in larger amounts or for longer than you’re meant to; spending a lot of time getting, using, or recovering from use of the substance; not managing to do what you should at work, home, or school because of substance use; continuing to use, even when it causes problems in relationships; giving up important social, occupational, or recreational activities because of substance use and needing more of the substance to get the effect you want.
None of these apply to the use of nicotine on a regular, long-term basis. In fact, people use nicotine to help them in everyday activities like focusing on work. There is some evidence that nicotine might have a role to play in helping those with dementia.167
In the public mind, the word ‘addiction’ conjures up a life in chaos and ruin, where the drug becomes all-consuming, where family and friends, school, college or job, everything in the person’s life, takes second place behind securing the next dose which (in the case of illegal drugs) may also involve criminal activity.
But does this picture of misery and despair map across to the person who is ‘addicted’ to nicotine? Because as the clinical literature confirms, if there are no significant short or long-term effects from using nicotine, and if you take the cigarettes out of the equation by changing the nicotine delivery system, the somewhat heretical question becomes – what’s the problem with being ‘addicted’ to nicotine? In this specific context, should we even talk about ‘addiction’ at all? In the absence of serious clinical or societal harm, isn’t this just a pleasurable habit? In which case, does the concept of ‘addiction’ become more of a moral or ideological construct than one based in public health?168,169,170
‘Addiction’ to nicotine falls far short of the addiction criteria set out in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders.

This is an important point: in many countries where SNP are available, the law demands prominent warnings on packaging about addiction. But is this really a serious clinical issue? Or is it more an attempt to shame people who use nicotine into feeling guilty? Smokers often cite the guilt and shame of being ‘addicted’ to nicotine as a reason for trying to quit. People who say they want to stop smoking will sometimes object to switching to SNP as they identify a continued addiction to nicotine to be some sort of failure. But for the many people who are unable or unwilling to give up their use of nicotine, it would be invidious to allow guilt and shame about nicotine ‘addiction’ to inhibit quit or switch attempts using SNP.
***
For the many people who are unable or unwilling to give up their use of nicotine, it would be invidious to allow guilt and shame about nicotine ‘addiction’ to inhibit quit or switch attempts using SNP.
There should be no doubt that using a vaping device, a HTP or specific smokeless products presents substantially less risk to the smoker who wants to switch away from cigarettes, but who wants the nicotine experience unavailable through NRT. The hope was that all those involved in public health and tobacco control would regard this third way out of smoking as a welcome addition to existing anti-smoking interventions.
Unfortunately, the advent of SNP has provoked the opposite reaction. The public health imperative to reduce the disease and death toll from smoking has arguably been side-lined in favour of a moral crusade against nicotine. This playbook aims to sow confusion about the health benefits of SNP and conflates THR with long-standing attempts by the tobacco industry to influence tobacco control policy. In doing so, researchers and THR activists are smeared as functionaries of Big Tobacco.
- Signals Analytics, Inc. Accessed 17 June 2020.
- Moysidou, A. et al. (2016). Knowledge and Perceptions about Nicotine, Nicotine Replacement Therapies and Electronic Cigarettes among Healthcare Professionals in Greece. International Journal of Environmental Research and Public Health, 13(5). https://doi.org/10.3390/ijerph13050514
- Ratschen, E. et al. (2009). Tobacco dependence, treatment and smoke-free policies: a survey of mental health professionals’ knowledge and attitudes. General Hospital Psychiatry, 31(6), 576–582. https://doi.org/10.1016/j. genhosppsych.2009.08.003
- Ramesh Patwardhan, S., & Murphy, M. A. (2013). Survey of GPs’ understanding of tobacco and nicotine products. Drugs and Alcohol Today, 13(2), 119–150. https://doi.org/10.1108/DAT-02-2013-0010
- McNeill, A. et al. (2020). Vaping in England: 2020 evidence update summary (Research and Analysis). Public Health England (PHE). https://www.gov.uk/government/publications/vaping-in-england-evidence-update-march-2020/vaping-inengland- 2020-evidence-update-summary
- Ministry of Health v Philip Morris (New Zealand) Limited [2018] NZDC 4478. Available at http://www.districtcourts.govt.nz/ assets/unsecure/2018-03-27/2018-NZDC-4478-MOH-v-Morris.pdf
- Toxicological evaluation of novel heat-not-burn tobacco products – non-technical summary. (2017). UK Committee on Toxicity. https://cot.food.gov.uk/sites/default/files/heat_not_burn_tobacco_summary.pdf
- Statement on heat not burn tobacco products. (2017). UK Committee on Toxicity. https://cot.food.gov.uk/sites/default/files/ heat_not_burn_tobacco_statement.pdf
- Statement on heat not burn tobacco products. (2017). UK Committee on Toxicity. https://cot.food.gov.uk/sites/default/files/ heat_not_burn_tobacco_statement.pdf
- McNeill A, Brose LS, Calder R, Bauld L & Robson D. (2018). Evidence review of e-cigarettes and heated tobacco products 2018. A report commissioned by Public Health England. (p. 243). Public Health England. https://assets.publishing.service. gov.uk/government/uploads/system/uploads/attachment_data/file/684963/Evidence_review_of_e-cigarettes_and_ heated_tobacco_products_2018.pdf
- Bekki, K. et al. (2017). Comparison of Chemicals in Mainstream Smoke in Heat-not-burn Tobacco and Combustion Cigarettes. Journal of UOEH, 39(3), 201–207. https://doi.org/10.7888/juoeh.39.201
- Li, X. et al. (2019). Chemical Analysis and Simulated Pyrolysis of Tobacco Heating System 2.2 Compared to Conventional Cigarettes. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 21(1), 111–118. https://doi.org/10.1093/ntr/nty005
- Mallock, N. et al. (2018). Levels of selected analytes in the emissions of “heat not burn” tobacco products that are relevant to assess human health risks. Archives of Toxicology, 92(6), 2145–2149. https://doi.org/10.1007/s00204-018-2215-y
- Ed Stephens. (2018, June 16). Modelling the effects of user exposure to harmful emissions across the spectrum of nicotine delivery. Global Forum on Nicotine, Warsaw. https://gfn.net.co/downloads/2018/EdStephens.pdf
- Simonavicius, E. et al. (2019). Heat-not-burn tobacco products: a systematic literature review. Tobacco Control, 28(5), 582–594. https://doi.org/10.1136/tobaccocontrol-2018-054419
- Text and references supplied by Brad Rodu, Professor of Medicine at the University of Louisville, Kentucky.
- Rodu, B. (2014). For Smokers Only: How Smokeless Tobacco Can Save Your Life. Sumner Books.
- Fisher, M. T. et al. (2019). Smokeless tobacco mortality risks: an analysis of two contemporary nationally representative longitudinal mortality studies. Harm Reduction Journal, 16(1), 27. https://doi.org/10.1186/s12954-019-0294-6
- Rodu, B. (2016, July 20). Tobacco Truth: Is Snus Safer Than Dip or Chew? Health Effects of All Are Close to Zero. Tobacco Truth. https://rodutobaccotruth.blogspot.com/2016/07/is-snus-safer-than-dip-or-chewhealth.html
- Rodu, B. (2009, August 13). Tobacco Truth: Cancer Risks from Smokeless Tobacco Use: Next To Nil. Tobacco Truth. https://rodutobaccotruth.blogspot.com/2009/08/cancer-risks-from-smokeless-tobacco-use.html
- Rodu, B. (2009, August 19). Tobacco Truth: Heart Attack and Stroke Risks from Smokeless Tobacco Use: Next to Nil. Tobacco Truth. https://rodutobaccotruth.blogspot.com/2009/08/heart-attack-and-stroke-risks-from.html
- Royal College of Physicians of London Tobacco Advisory Group. (2002). Protecting Smokers, Saving Lives: The Case for a Tobacco and Nicotine Regulatory Authority. Royal College of Physicians.
- Nitzkin JL, Rodu B. (2008). The case for harm reduction for control of tobacco-related illness and death. Resolution and White Paper. American Association of Public Health Physicians; Wayback Machine. https://web.archive.org/ web/20100510170828/http://www.aaphp.org/special/joelstobac/20081026HarmReductionResolutionAsPassedl.pdf
- Gakidou, E. et al. (2017). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 390(10100), 1345–1422. https://doi.org/10.1016/S0140-6736(17)32366-8
- While fewer women than men smoke cigarettes, in parts of India, for example, there are high rates of head and neck cancer among low income women using smokeless tobacco products.
- Carlsson, S. et al. (2017). Smokeless tobacco (snus) is associated with an increased risk of type 2 diabetes: results from five pooled cohorts. Journal of Internal Medicine, 281(4), 398–406. https://doi.org/10.1111/joim.12592
- Rasouli, B. et al. (2017). Use of Swedish smokeless tobacco (snus) and the risk of Type 2 diabetes and latent autoimmune diabetes of adulthood (LADA). Diabetic Medicine: A Journal of the British Diabetic Association, 34(4), 514–521. https://doi. org/10.1111/dme.13179
- Lee, P. N. (2011). Summary of the epidemiological evidence relating snus to health. Regulatory Toxicology and Pharmacology: RTP, 59(2), 197–214. https://doi.org/10.1016/j.yrtph.2010.12.002
- Araghi, M. et al. (2017). Use of moist oral snuff (snus) and pancreatic cancer: Pooled analysis of nine prospective observational studies. International Journal of Cancer, 141(4), 687–693. https://doi.org/10.1002/ijc.30773
- Hansson, J. et al. (2009). Use of snus and risk for cardiovascular disease: results from the Swedish Twin Registry. Journal of Internal Medicine, 265(6), 717–724. https://doi.org/10.1111/j.1365-2796.2009.02081.x
- WHO Study Group on Tobacco Product Regulation. (2010). Report on the Scientific Basis of Tobacco Product Regulation (No. 955). WHO. https://www.who.int/tobacco/global_interaction/tobreg/publications/tsr_955/en/
- Scientific Committee on Emerging and Newly Identified Health Risks. Health effects of smokeless tobacco products. Health and Consumer Protection Directorate, European Commission, 2008. Available at ec.europa.eu/health/ph_risk/ committees/04_scenihr/docs/scenihr_o_013.pdf
- See also O’Leary, R., & Polosa, R. (2020). Tobacco harm reduction in the 21st century. Drugs and Alcohol Today, ahead-ofprint( ahead-of-print). https://doi.org/10.1108/DAT-02-2020-0007
- Blount, B. C. et al. (2019). Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI. New England Journal of Medicine, 382(8), 697–705. https://doi.org/10.1056/NEJMoa1916433
- Downs, D. et al. (2019, September 24). Journey of a Tainted Vape Cartridge: from China’s labs to your lungs. A Leafly Investigation. Leafly. https://www.leafly.com/news/politics/vape-pen-injury-supply-chain-investigation-leafly
- Downs, D. (2019, September 11). Vape Pen Lung Disease: Vitamin E Oil Explained. Leafly. https://www.leafly.com/news/ health/vape-pen-lung-disease-vitamin-e-oil-explained
- Note that devices produced for vaping nicotine e-liquid are not suitable for vaping THC. The reason the products are incompatible is that e-liquid atomisers are designed for the relatively thin PG/VG e-liquid mixture, and cannabis oil atomizers are specifically made to vaporise ultra-thick THC oil. The coils and wicks of one will not handle the substance meant for use in the other.
- Jim McDonald. (2020, May 8). A Look Back at CDC’s Award-Nominated “EVALI” Response. Vaping360. https://vaping360. com/vape-news/90032/a-look-back-at-cdcs-award-nominated-evali-response/
- Hall, W. et al. (2020). Lessons from the public health responses to the US outbreak of vaping-related lung injury. Addiction (Abingdon, England). https://doi.org/10.1111/add.15108
- Gartner, C. et al. (2020). Miscommunication about the causes of the US outbreak of lung diseases in vapers by public health authorities and the media. Drug and Alcohol Review, 39(1), 3–6. https://doi.org/10.1111/dar.13024
- CDC’s Office on Smoking and Health. (2020, February 25). Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/basic_ information/e-cigarettes/severe-lung-disease.html
- Polosa, R. et al. (2019). The effect of e-cigarette aerosol emissions on respiratory health: a narrative review. Expert Review of Respiratory Medicine, 13(9), 899–915. https://doi.org/10.1080/17476348.2019.1649146
- RCP policy: public health and health inequality. (2016). Nicotine without smoke: Tobacco harm reduction. Royal College of Physicians. https://www.rcplondon.ac.uk/projects/outputs/nicotine-without-smoke-tobacco-harm-reduction, p. 58
- Smoking: harm reduction (Guidance No. PH45; Public Health Guideline). (2013). National Institute for Health and Care Excellence (NICE). https://www.nice.org.uk/Guidance/PH45
- Mayer, B. (2014). How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious selfexperiments in the nineteenth century. Archives of Toxicology, 88(1), 5–7. https://doi.org/10.1007/s00204-013-1127-0
- IARC. (2004). Tobacco Smoke and Involuntary Smoking. World Health Organisation International Agency for Research on Cancer. https://publications.iarc.fr/Book-And-Report-Series/Iarc-Monographs-On-The-Identification-Of-Carcinogenic- Hazards-To-Humans/Tobacco-Smoke-And-Involuntary-Smoking-2004
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. (2014). The Health Consequences of Smoking – 50 Years of Progress: A Report of the Surgeon General. Centers for Disease Control and Prevention (US). http://www.ncbi.nlm.nih.gov/books/NBK179276/
- Polosa, R. et al. (2014). Effect of Smoking Abstinence and Reduction in Asthmatic Smokers Switching to Electronic Cigarettes: Evidence for Harm Reversal. International Journal of Environmental Research and Public Health, 11(5), 4965–4977. https://doi.org/10.3390/ijerph110504965
- Polosa, R. et al. (2018). Health effects in COPD smokers who switch to electronic cigarettes: a retrospective-prospective 3-year follow-up. International Journal of Chronic Obstructive Pulmonary Disease, 13, 2533–2542. https://doi.org/10.2147/ COPD.S161138
- George, J. et al. (2019). Cardiovascular Effects of Switching From Tobacco Cigarettes to Electronic Cigarettes. Journal of the American College of Cardiology, 74(25), 3112–3120. https://doi.org/10.1016/j.jacc.2019.09.067
- Polosa, R. et al. (2016). Evidence for harm reduction in COPD smokers who switch to electronic cigarettes. Respiratory Research, 17(1), 166. https://doi.org/10.1186/s12931-016-0481-x
- Miler, J. A., & Mayer, B. (2016). Changes in the Frequency of Airway Infections in Smokers Who Switched To Vaping: Results of an Online Survey. Journal of Addiction Research & Therapy, 7. https://doi.org/10.4172/2155-6105.1000290
- Olmedo Pablo et al. (n.d.). Metal Concentrations in e-Cigarette Liquid and Aerosol Samples: The Contribution of Metallic Coils. Environmental Health Perspectives, 126(2), 027010. https://doi.org/10.1289/EHP2175
- Farsalinos, K. E., & Rodu, B. (2018). Metal emissions from e-cigarettes: a risk assessment analysis of a recently-published study. Inhalation Toxicology, 30(7–8), 321–326. https://doi.org/10.1080/08958378.2018.1523262
- Farsalinos, K. E. et al. (2015). Evaluation of Electronic Cigarette Liquids and Aerosol for the Presence of Selected Inhalation Toxins. Nicotine & Tobacco Research, 17(2), 168–174. https://doi.org/10.1093/ntr/ntu176
- Ward, A. et al. (2020). Electronic nicotine delivery system design and aerosol toxicants: A systematic review. PLOS ONE, 15, e0234189. https://doi.org/10.1371/journal.pone.0234189
- Stephens, W. E. (2018). Comparing the cancer potencies of emissions from vapourised nicotine products including e-cigarettes with those of tobacco smoke. Tobacco Control, 27(1), 10–17. https://doi.org/10.1136/ tobaccocontrol-2017-053808
- Burstyn, I. (2014). Peering through the mist: systematic review of what the chemistry of contaminants in electronic cigarettes tells us about health risks. BMC Public Health, 14(1), 18. https://doi.org/10.1186/1471-2458-14-18
- Polosa, R. et al. (2017). Health impact of E-cigarettes: A prospective 3.5-year study of regular daily users who have never smoked. Scientific Reports, 7. https://doi.org/10.1038/s41598-017-14043-2
- Lusignan, S. de et al. (2020). Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre primary care network: a cross-sectional study. The Lancet Infectious Diseases, 0(0). https://doi.org/10.1016/S1473-3099(20)30371-6
- Clive Bates. (2020, June 1). The Unlikely Savior? Smoking, nicotine and COVID-19: What is going on? Tobacco Reporter. https://tobaccoreporter.com/2020/06/01/the-unlikely-savior/
- Joe Gitchell. (2020, June 14). The Odd Case of Tobacco, Nicotine, and COVID-19. ConscienHealth. https://conscienhealth. org/2020/06/the-odd-case-of-tobacco-nicotine-and-covid-19/
- Farsalinos, K. et al. (2020). Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis: Therapeutic Advances in Chronic Disease. https://doi. org/10.1177/2040622320935765
- A recent UK study of over 8 million patients investigated whether certain drugs used in the treatment of heart problems might put patients at increased risk of contracting COVID-19 and subsequent admission to intensive care. Among a whole range of risk variables studied, the authors concluded that, “there was a small increased risk of both adverse outcomes among ex-smokers compared with never-smokers. The apparent protective association was greatest for heavy and moderate smokers and most markedly on the risk of ICU admission which was 88 per cent lower in heavy smokers compared with non-smokers”. Hippisley-Cox, J. et al. (2020). Risk of severe COVID-19 disease with ACE inhibitors and angiotensin receptor blockers: cohort study including 8.3 million people. Heart. https://doi.org/10.1136/ heartjnl-2020-317393
- St Helen, G. et al. (2016). Nicotine delivery, retention and pharmacokinetics from various electronic cigarettes. Addiction (Abingdon, England), 111(3), 535–544. https://doi.org/10.1111/add.13183
- Samburova, V. et al. (2018). Aldehydes in Exhaled Breath during E-Cigarette Vaping: Pilot Study Results. 6, 1–14. https:// doi.org/10.3390/toxics6030046
- For example, Glantz, S. A., & Bareham, D. W. (2018). E-Cigarettes: Use, Effects on Smoking, Risks, and Policy Implications. Annual Review of Public Health, 39, 215–235. https://doi.org/10.1146/annurev-publhealth-040617-013757
- David, G. et al. (2020). Tracing the composition of single e-cigarette aerosol droplets in situ by laser-trapping and Raman scattering. Scientific Reports, 10(1), 7929. https://doi.org/10.1038/s41598-020-64886-5
- Lampos, S. et al. (2019). Real-Time Assessment of E-Cigarettes and Conventional Cigarettes Emissions: Aerosol Size Distributions, Mass and Number Concentrations. Toxics, 7(3), 45. https://doi.org/10.3390/toxics7030045
- Zhao, T. et al. (2017). Characteristics of secondhand electronic cigarette aerosols from active human use. Aerosol Science and Technology, 51(12), 1368–1376. https://doi.org/10.1080/02786826.2017.1355548
- Scungio, M. et al. (2018). Measurements of electronic cigarette-generated particles for the evaluation of lung cancer risk of active and passive users. Journal of Aerosol Science, 115, 1–11. https://doi.org/10.1016/j.jaerosci.2017.10.006
- Avino, P. et al. (2018). Second-hand aerosol from tobacco and electronic cigarettes: Evaluation of the smoker emission rates and doses and lung cancer risk of passive smokers and vapers. Science of The Total Environment, 642, 137–147. https://doi.org/10.1016/j.scitotenv.2018.06.059
- McNeill A, Brose LS, Calder R, Bauld L & Robson D. (2018). Evidence review of e-cigarettes and heated tobacco products 2018. A report commissioned by Public Health England. (p. 243). Public Health England. https://assets.publishing.service. gov.uk/government/uploads/system/uploads/attachment_data/file/684963/Evidence_review_of_e-cigarettes_and_ heated_tobacco_products_2018.pdf
- Glasser, A. M. et al. (2017). Overview of Electronic Nicotine Delivery Systems: A Systematic Review. American Journal of Preventive Medicine, 52(2), e33–e66. https://doi.org/10.1016/j.amepre.2016.10.036
- Zwack, L. M. et al. (2017). Evaluation of Chemical Exposures at a Vape Shop (Health Hazard Evaluation Report 2015- 0107-3279; p. 30). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. https://www.cdc.gov/niosh/hhe/reports/pdfs/2015-0107-3279.pdf
- Glasser, A. M. et al. (2020). Youth Vaping and Tobacco Use in Context in the United States: Results from the 2018 National Youth Tobacco Survey. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. https://doi.org/10.1093/ntr/ntaa010
- For more detailed information about US teen vaping including the significant but largely ignored increase in teens vaping
THC contrasted with dramatic falls in teen smoking, go to:
Rodu, B. (2020, January 10). Tobacco Truth: 2019 NYTS Data Reveals Teen Vaping Up, Smoking Eradication Within Reach. Tobacco Truth. https://rodutobaccotruth.blogspot.com/2020/01/2019-nyts-data-reveals-teen-vaping-up.html
Historical NYTS Data and Documentation | CDC. (2019, December 17). https://www.cdc.gov/tobacco/data_statistics/ surveys/nyts/data/index.html
Siegel, M. (2020, January 26). The Rest of the Story: Tobacco and Alcohol News Analysis and Commentary: CDC is Concealing and Suppressing Information on Youth Marijuana Vaping to Over-hype Harms of E-Cigarettes. The Rest of the Story. https://tobaccoanalysis.blogspot.com/2020/01/cdc-is-concealing-and-suppressing.html - Use of e-cigarettes among young people in Great Britain, 2019. (2019, June 18). Action on Smoking and Health. https://ash.org.uk/information-and-resources/fact-sheets/statistical/use-of-e-cigarettes-among-young-people-in-greatbritain- 2019/
- Levy, D. T. et al. (2019). Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tobacco Control, 28(6), 629–635. https://doi.org/10.1136/tobaccocontrol-2018-054446
- Kim, S., & Selya, A. S. (2020). The Relationship Between Electronic Cigarette Use and Conventional Cigarette Smoking Is Largely Attributable to Shared Risk Factors. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 22(7), 1123–1130. https://doi.org/10.1093/ntr/ntz157
- Interestingly, the CDC’s Youth Risk Behaviour Survey for 2017 showed past-30-day cannabis use by high school students at 19.8 per cent, nearly the same as vaping among the same group but with none of the same moral panic. YRBSS | Youth Risk Behavior Surveillance System | Data | Adolescent and School Health | CDC. (2020, August 20). https://www.cdc.gov/ healthyyouth/data/yrbs/index.htm
- Some claims derive from rodent studies which are generally a very poor proxy for real life health risks in humans. Buck, S. (2016, April 8). Why Journalists Should Stop Publishing Studies Conducted With Mice. Arnold Foundation. https://www.arnoldventures.org/stories/stop-publishing-mouse-studies/
- Stop smoking services in England have been hit by significant cuts to public health funding. Services on offer vary across the country, but many are ‘vape-friendly’. Many ways forward. (2020, January 14). Action on Smoking and Health. https://ash.org.uk/information-and-resources/reports-submissions/reports/many-ways-forward/
- O’Leary, R., & Polosa, R. (2020). Tobacco harm reduction in the 21st century. Drugs and Alcohol Today, ahead-of-print( ahead-of-print). https://doi.org/10.1108/DAT-02-2020-0007
- A Changing Landscape: Stop Smoking Services and Tobacco Control in England. (2019). Cancer Research UK and Action on Smoking and Health (ASH). http://ash.org.uk/wp-content/uploads/2019/03/2019-LA-Survey-Report.pdf
- Hajek, P. et al. (2019). E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technology Assessment (Winchester, England), 23(43), 1–82. https://doi.org/10.3310/hta23430. For other studies concluding that vaping aids smoking cessation, see also; Brown, J. et al. (2014). Real-world effectiveness of e-cigarettes when used to aid smoking cessation: a cross-sectional population study. Addiction, 109(9), 1531–1540. https://doi.org/10.1111/add.12623; Jackson, S. E. et al. (2019). Moderators of real-world effectiveness of smoking cessation aids: a population study. Addiction, 114(9), 1627–1638. https://doi.org/10.1111/add.14656; Walker, N. et al. (2020). Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. The Lancet Respiratory Medicine, 8(1), 54–64. https://doi.org/10.1016/S2213-2600(19)30269-3.
- Novotny, T. E., & Schalkwyk, M. C. I. van. (2020). How Should Physicians in Low- and Middle-Income Countries Regard Electronic Nicotine Delivery Systems to Facilitate Smoking Cessation? AMA Journal of Ethics, 22(2), 82–92. https://doi. org/10.1001/amajethics.2020.82.
- Sarma Smitha et al. (2017). Availability, Sales, and Affordability of Tobacco Cessation Medicines in Kerala, India. Circulation: Cardiovascular Quality and Outcomes, 10(11), e004108. https://doi.org/10.1161/CIRCOUTCOMES.117.004108
- Glover, M., & Phillips, C. V. (2020). Potential effects of using non-combustible tobacco and nicotine products during pregnancy: a systematic review. Harm Reduction Journal, 17. https://doi.org/10.1186/s12954-020-00359-2
- Iq’mik or blackbull is a smokeless product made using a mixture of tobacco and the ash of a fungus Phellinus igniarius, also known as punk ash. It is popular among First Nation Alaskans who believe this product is healthier than USstyle dipping tobacco. They may be right, as a related fungus Phellinus Linteus is reputed to convey several health benefits. Wong, C. (2020, April 28). The Health Benefits and Uses for Phellinus Linteus. Verywell Health. https://www. verywellhealth.com/the-benefits-of-phellinus-linteus-88684
- Support to Quit Smoking in Pregnancy. (2019). The Royal College of Midwives. https://www.rcm.org.uk/publications/ position-statements/support-to-quit-smoking-in-pregnancy/
- See Ronald K. Siegel Ph.D. (2005). Intoxication: The Universal Drive for Mind-Altering Substances (3 edition). Park Street Press. The author details how not only humans throughout history, but also animals seek to alter their state of consciousness.
- RCP policy: public health and health inequality. (2016). Nicotine without smoke: Tobacco harm reduction. Royal College of Physicians. https://www.rcplondon.ac.uk/projects/outputs/nicotine-without-smoke-tobacco-harm-reduction
- Interestingly, researchers from Liverpool University have concluded that this type of categorisation of mental health problems is essentially meaningless in many real world situations where conditions might overlap and where not all human distress can be conveniently labelled as a ‘disorder’ where the notion of what is ‘normal’ is subjective. Anderer, J. (2019, July 9). Study: Psychiatric Diagnoses Are ‘Scientifically Meaningless’ In Treating Mental Health. Study Finds. https:// www.studyfinds.org/study-psychiatric-diagnoses-are-scientifically-meaningless/
- As an interesting aside, there is evidence that nicotine might be more ‘addictive’ when smoked in cigarettes because of other additives in the smoke to aid nicotine delivery and absorption, including MAO inhibitors, sugars and polysaccharides. RCP policy: public health and health inequality. (2016). Nicotine without smoke: Tobacco harm reduction. Royal College of Physicians. https://www.rcplondon.ac.uk/projects/outputs/nicotine-without-smoke-tobacco-harm-reduction, p.61
- Some clinicians prefer ‘dependence’ to ‘addiction’ and would argue that nicotine ‘enjoyment’ is simply a manifestation of dependence, keeping the regular use of nicotine within a medical context.
- It has also been proposed that reframing smoking as an ‘addiction’ rather than a ‘habit’ opened the door to the ‘medicalisation’ of smoking and a route into a burgeoning and hugely profitable public health issue by the pharmaceutical industry.
